Choosing the right Interlocking nail implant for surgical procedures is a critical decision. Dr. John Anderson, a renowned orthopedic surgeon, emphasizes, "Selecting the right implant can make all the difference in recovery." Interlocking nail implants are designed to stabilize fractures. However, not all implants are created equal.
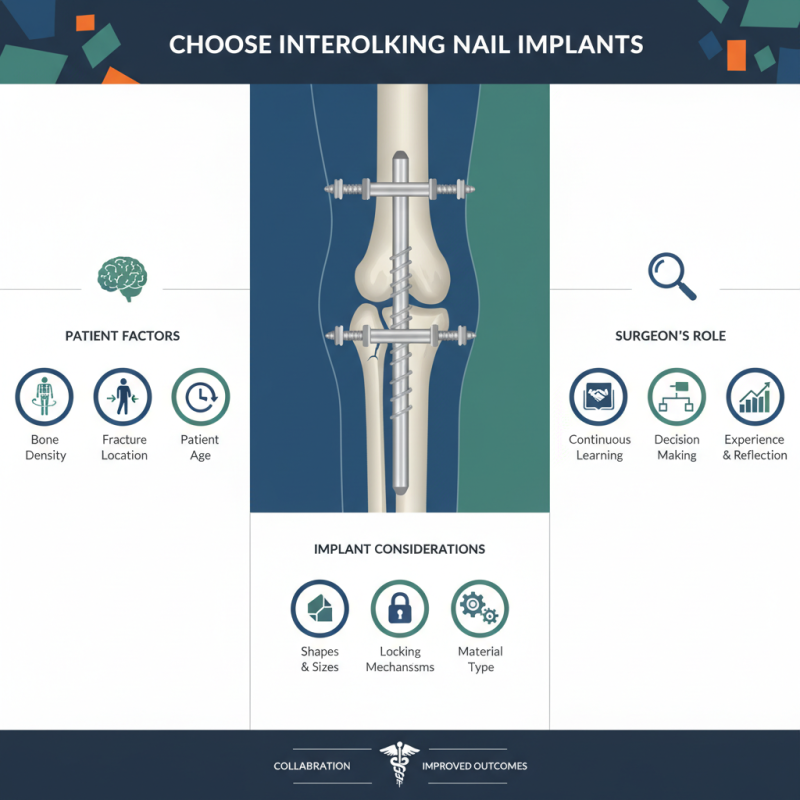
Surgeons must consider multiple factors before making a choice. Bone density, fracture location, and patient age play a role. Dr. Anderson notes, "Each patient is unique; their needs dictate the implant." This adds a layer of complexity to the selection process. Sometimes, even experienced surgeons face challenges with available options.
Interlocking nail implants can have varying shapes, sizes, and locking mechanisms. A mismatch can lead to complications or prolonged recovery. It's vital for surgeons to acknowledge their limitations. Continuous learning and adapting to new technologies in the field are essential. Reflection on past cases often unveils lessons that guide future decisions. The right interlocking nail implant can significantly enhance treatment outcomes.
Interlocking nail implants are surgical tools used to stabilize fractures, particularly in long bones. They provide internal support during healing. This method allows for early mobilization, which can be crucial for recovery. The implant is inserted into the medullary canal of a bone. It is designed to hold fractured parts together, ensuring proper alignment during healing.
Surgeons often choose interlocking nails for their versatility. They are effective in treating complex fractures and can accommodate various angles. The design also helps in distributing stresses evenly across the bone. However, selecting the right implant is not always straightforward. Factors such as the location of the fracture and the patient’s anatomy play a critical role. Sometimes, the wrong choice can lead to complications, which is a significant risk.
Understanding the specific needs of the surgery is essential for success. A careful evaluation of the fracture type is necessary. Sometimes, additional imaging might be needed. Surgeons face tough decisions here. They must weigh benefits against potential drawbacks. This process requires experience and insight, but it is crucial for optimal patient outcomes.
Choosing the right interlocking nail implant for surgery involves careful consideration of material and design. The implant's material affects its strength and biocompatibility. Common materials include titanium and stainless steel. Titanium is lightweight and corrosion-resistant. It integrates well with bone. On the other hand, stainless steel is often more affordable but can be heavier. Each material has its pros and cons.
Design is equally crucial. Consider the shape and locking mechanism of the nail. Some designs feature advanced locking options. These can provide better stability during healing. Others may have a more straightforward design but could compromise stability. Think about the specific needs of the patient's injury when evaluating designs.
Choosing the right interlocking nail implant for surgery can significantly affect patient outcomes. Patient-specific factors are essential in determining the best implant option. A thorough evaluation of these factors can lead to improved healing and reduced complications. Studies show that tailoring the implant to patient anatomy enhances fixation strength by 20-30%.
Bone quality is one crucial factor to assess. Patients with osteoporotic bone may require different implant specifications compared to healthy individuals. A recent report indicated that almost 60% of patients with osteoporosis experienced complications during standard implant procedures. Surgeons must consider such variations in bone density and structure during the decision-making process.
Tips: Always perform a comprehensive imaging assessment to understand bone geometry. Also, involve the patient in discussions about implant options. This builds trust and can lead to better decisions. Remember, even minor miscalculations can lead to significant issues post-surgery. Monitor the biomechanical properties of the chosen implant to ensure it meets individual needs. Each patient's anatomy is unique, and an average approach might not suffice.
Interlocking nail implants represent a significant advancement in surgical technology. Recent studies indicate a growing adoption of these devices in orthopedic surgeries. The market for interlocking nails is expected to reach over $1 billion by 2025, reflecting a compound annual growth rate of 7.5%. This indicates a robust demand for innovative solutions in fracture fixation.
Current trends highlight minimal invasive techniques and enhanced biocompatibility. Surgeons are increasingly choosing materials that integrate seamlessly with bone tissue, such as titanium alloys. These innovations reduce recovery times and complications. However, challenges remain. Some implants may lead to complications, such as infection or failure to fuse.
Recent reports show that approximately 15% of interlocking nail surgeries result in complications. This necessitates careful preoperative assessments. Surgeons must consider each patient's unique anatomy. A tailored approach can improve outcomes. Investing in advanced imaging technologies can aid in selecting the correct implant size. Yet, with the rapid pace of innovation, ongoing education remains crucial for surgical teams.
| Implant Type | Material | Indication | Advantages | Current Trend |
|---|---|---|---|---|
| Standard Interlocking Nail | Titanium | Femur & Tibia Fractures | High strength, Biocompatible | Minimal invasive techniques |
| Magnetic Intramedullary Nail | Stainless Steel | Non-union Fractures | Non-invasive lengthening, Adjustable | Smart technology integration |
| Locking Compression Plate Nail | Titanium Alloy | Complex Fractures | Stable fixation, Enhanced healing | Improved fixation techniques |
| Functionally Graded Materials Nail | Composite Materials | Bone regeneration | Optimized mechanical properties, Flexibility | Personalized implants |
When selecting an interlocking nail implant for surgery, understanding clinical outcomes is crucial. Recent studies indicate that success rates vary widely among different types of implants. For example, a meta-analysis published in 2022 reported an overall success rate of approximately 85% for interlocking nails. This percentage changes based on the specific implant design and the fracture type being treated. Notably, some designs may yield lower success rates, around 70%, particularly in complex femoral fractures.
Complications can also arise, influencing the decision-making process. Data suggests that nearly 15% of patients experience complications like infection or non-union. The rates differ based on surgical technique and the patient's health status. Complications can lead to additional surgeries, which complicates recovery. Surgeons must weigh these risks against the expected benefits when selecting an implant.
While many patients recover well, there are those who face challenges. Some may experience persistent pain or reduced mobility post-surgery. Understanding these risks is essential for comprehensive patient education. Surgeons will benefit from being informed about the latest research and outcomes, as this can lead to better patient care. Data-driven decisions can improve the chances of successful recovery.
This chart presents the success rates and complications of various interlocking nail implants used in surgery. The data highlights the effectiveness and safety of different implants based on clinical outcomes.
Update your browser to view this website correctly. Update my browser now
